 LETTERKENNY General Hospital has extended its complete ban on visitors to the site due to spread of a virus.
LETTERKENNY General Hospital has extended its complete ban on visitors to the site due to spread of a virus.
The HSE says that due to the presence of the Winter Vomiting Bug, no visitors will be allowed to visit the hospital at this time to help curtail the spread of infection.
“There will be allowances made for the maternity department where fathers will be allowed to visit,” said a spokeswoman.
“In cases where a patient is critically ill, a nominated next of kin should ring the ward in advance to make arrangements to visit.
“All appropriate infection control measures are being taken to deal with the situation at the hospital at the moment and the ban on visiting will remain in place until the wards are free from the outbreak. We are appealing to the public to adhere strictly to the ban on visiting.”
She said that Letterkenny General Hospital wishes to thank patients and the public for their cooperation and apologise for any inconvenience caused.
FURTHER INFORMATION
Vomiting bug increase – public can help stop the spread
The HSE Health Protection Surveillance Centre (HPSC) has asked members of the public to respect hospital visit restrictions and to follow hand hygiene directions when visiting patients following a recent increase in winter vomiting bug cases.
One hundred and ninety cases of winter vomiting bug, also known as norovirus, were notified to HPSC during the week before last, while a further 115 cases were notified last week according to HPSC specialist in public health medicine, Dr Paul McKeown. “In addition, we have been getting numerous reports of outbreaks affecting hospitals, nursing homes and hotels around the country.”
“In a normal week 50 cases would be regarded as high number of notifications so we are in an upsurge period.
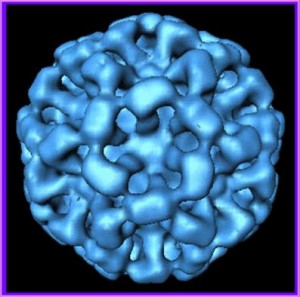
“Norovirus is the gastrointestinal equivalent of the common cold. In any year at least 1% – and in high activity years up to 5% – of the population can expect to be affected by this virus meaning that between 1,000 and 5,000 people could fall ill with norovirus per week during a busy period.
“Members of the public can help stop the spread of illness by respecting hospital and nursing home visitor restrictions and by using the alcohol gel supplied as they enter and leave the facilities. While Out Patient Departments and Emergency Departments are not affected, patients are asked not to attend hospital if they have been affected by vomiting and/or diarrhoea in the last 48 hours. Handwashing with soap and water – especially after contact with someone who is ill and after using the toilet – is also extremely important, particularly if you are or have been sick.
“When it gets into hospitals or nursing homes, it can cause serious disruption, for example ward closures, cancelled operations and added pressure on emergency departments. It is important that ill and vulnerable patients in these settings do not become more ill than they already are.
“Norovirus is highly infectious and very resilient. It is capable of spreading from person-to-person, by food and water, via surfaces and through the air. It can survive for a number of weeks in the environment and on surfaces such as door handles, toilet pulls, TV remote controls, light switches or worktops.
“Norovirus does not usually cause serious illness, but it is very easily spread. People who contract it can be infectious for 48 hours after they recover. The principal symptoms are nausea, vomiting and diarrhoea and generally begin very suddenly with nausea followed by projectile vomiting. A little later watery diarrhoea may develop as well.
“Symptoms will usually last only a day or two but can, occasionally last longer. If you are concerned (e.g. prolonged vomiting/diarrhoea especially in small children and elderly people), telephone your GP for advice¸ to reduce the possibility of bringing norovirus into the GP surgery.
“The exact numbers of cases currently in Ireland is not known as many people will recover at home without seeking medical attention. Cases have been recorded in a number of hospitals and hotels around the country in the last two or three weeks. Hospitals have infection control measures in place to limit the spread of the virus which can include visitor restrictions.
“The most important steps in reducing the impact of Norovirus in healthcare settings are to keep it out of the hospital, to immediately clean any contaminated areas, to exercise good hand hygiene and to segregate those who are ill.
“Without the cooperation of the public this virus can spread very quickly throughout nursing homes and hospitals, causing discomfort to patients and disruption to services. To reduce the likelihood of spread of norovirus it is important to remember the following:
· If you have recently had vomiting / diarrhoea, do not visit a hospital or nursing home until you have been well for 48 hours.
· If your child has had vomiting / diarrhoea, they should not go to school/crèche until they have been well for 48 hours.
“The following advice will help stop spread of Norovirus at home and in the community:
· At home, wash your hands regularly after using the toilet and when touching food
· If someone vomits at home, use hot water and detergent to clean up any soiling and wash your hands thoroughly after
· If you are sick you should remain off work until you have been well for 48 hours
· There is no specific treatment for norovirus apart from sipping plenty of clear fluids such as water or flat lemonade.
Further information on protecting yourself, your family and your business from the threat of norovirus can be found on the HPSC’s website at www.hpsc.ie/hpsc/A-Z/Gastroenteric/Norovirus/ , added Dr McKeown.